Closing the Health Inequity Gap by Investing in Data and Technology
UNICEF and The Rockefeller Foundation teamed up to strengthen community-based primary health systems in Eastern and Southern Africa by equipping health workers with data-driven tools that enable the delivery of high-quality interventions and support real-time reporting.
Though the world has significantly reduced neonatal and maternal deaths, newborns and mothers — including adolescent mothers — continue to perish in devastating numbers. In 2021, 5 million children under age 5 died. In that same year, roughly 800 women a day died from causes related to pregnancy or childbirth. These outcomes are often preventable or treatable through localized approaches to deliver quality, accessible and affordable health care. Addressing the compounding effects of poverty, malnutrition, the worsening climate crisis, ongoing conflicts and displacements on child and maternal health requires bold, innovative action.
Advances in digital technology and data science show promise in enhancing the delivery of essential care to improve maternal, newborn and child health outcomes. Technological innovations in health care must be scaled and designed to be sustainable by local governments and organizations to reach the people who need them most. UNICEF and longtime partner The Rockefeller Foundation recently completed an initiative to strengthen community-based primary health care by improving timely access to and use of community-level data, including equipping community health workers (CHWs) with data-driven tools to make timely and lifesaving health care decisions that enable the delivery of high-quality community-based interventions and support real-time reporting.
The Intelligent Community Health Systems (iCoHS) project supported countries in implementing and owning scalable, data-driven community-based primary health care with an equity focus on the most deprived populations. Launched in 2019 with the creation of innovation and learning labs in Uganda and India, the project later expanded to Burundi, Eritrea, Ethiopia, Madagascar, Malawi, Mozambique, Rwanda, Somalia, Tanzania/Zanzibar and Zambia.
Empowering community health workers
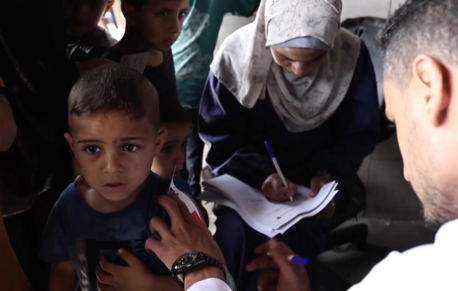
The iCoHS initiative aimed to expand the reach and strengthen the capacity of CHWs to deliver essential health services. In many populations, CHWs are the first to provide preventive, promotive and basic curative care and to ensure the continuity of essential health and nutrition services during pandemics and climate shocks. CHWs frequently identify and respond to potential disease outbreaks as well.
Often, CHWs, who are mostly women, are overburdened with responsibility for many households across large territories. They must also balance their patient care with administrative work, including reporting information to a national or primary health system. Data and technology advances can greatly ease the burdens placed on these vital workers.
Community health workers – 70% of whom are women - are crucial to delivering last-mile care & building trust. @MinofHealthUG + @UNICEF have partnered w. CHWs in Uganda to improve family health using digital tools. Learn more 👇#WD2023pic.twitter.com/oxi8zT4EmW
— The Rockefeller Foundation (@RockefellerFdn) July 19, 2023
Enhancing community health systems in Uganda
UNICEF and The Rockefeller Foundation have long supported strengthening community health systems and integrating CHWs into formal health systems. In Uganda, iCoHS provided direct financial and technical support to the Ministry of Health’s (MoH’s) design and implementation of a National Community Health Strategy.
The iCoHS project supplied CHWs, known as Village Health Teams (VHTs) in Uganda, with digital solutions to streamline the decision-making process in the field and capture and share data that unblock health system bottlenecks and facilitate resource allocation to the greatest need.
The MoH’s Division of Health Information, along with a consortium of partners convened by UNICEF, analyzed bottlenecks in the health system and identified impediments to optimal community-level service delivery that could benefit from digital health solutions. The analysis shaped the design of an electronic community health information system (eCHIS) piloted in the country’s Lamwo and Ntungamo districts. The two disparate regions allowed the tool to be tested under different demographic and developmental conditions.
In the past, a VHT would determine a course of treatment during an assessment of a child, which often led to mistakes and delays in care. Using the new tool, “The VHT will enter what the child is feeling — the signs, the conditions, and the symptoms, and … the tool will summarize what to give this child,” explains Roland Nahabwe, a health assistant in Uganda’s Ntumgamo district.

Implementing and owning solutions at the local level
The project team trained 500 VHTs and 16 district supervisors to capture and transmit data via a smartphone app to Uganda’s primary health system. The eCHIS helps VHTs assess, diagnose, treat and refer patients, and conduct disease surveillance. Policymakers and VHTs now have near real-time monitoring to facilitate more rapid decision-making and interventions.
Notably, the phones use a solar charger or power bank and work in regions with little or no access to electricity. By 2024, the MoH plans to scale community digital tools to more than 17,000 VHTs, which will enable data-driven decision-making for countless communities.
The eCHIS platform improved delivery and access to primary care in Uganda and has helped to institutionalize community health systems within the primary health care system — addressing a significant objective of the MoH’s National Community Health Strategy. Nahabwe describes the improvement: “We report timely. We know where the problem in the community is, and we intervene timely.” Lessons learned in the iCoHS implementation informed the National Health Information and Digital Health Strategy development, further reinforcing and strengthening governance in the digital health space.
Investing in country-led community health programs
Equitable access to primary health care requires decision-making based on accurate and timely health data. However, national community health programs often lack sufficient funding. The Rockefeller Foundation and UNICEF collaboration with the Ugandan MoH has catalyzed other donors to strengthen the health data ecosystem, including the Johnson & Johnson Foundation, ELMA Philanthropies and the Global Fund. Buoyed by the success of the national community health strategy launch, MoH will direct these new investments to its ongoing optimization of community-based primary health care. Increased demand for and use of community information is driving health system responsiveness and accountability and, ultimately, improving the quality and reach of care.

Investment in scalable, sustainable national health systems is imperative to countries that hope to meet the UN Sustainable Development Goals, particularly SDG 3, to ensure healthy lives and promote well-being for all at all ages. UNICEF supports the Monrovia Call to Action, which calls on countries “to fund, scale and strengthen community health programs as an integral part of primary health care for the realization of universal health coverage.” The iCoHS project addressed key objectives in Uganda’s MoH Community Health Roadmap and exemplifies The Rockefeller Foundation and UNICEF’s shared commitment to dismantling systemic health care inequities to reduce maternal and child mortality. “I see the life of these children improved,” says Nahabwe in Uganda. “Now when these children are not getting sick due to pneumonia, due to malaria, due to diarrhea, children will not be stunted…. I see this program is taking us very far as a country.”
With over three years of technical and financial support from The Rockefeller Foundation, through a truly collaborative, adaptive partnership, countries, communities and CHWs continue to benefit from iCoHS. The Rockefeller Foundation is also a founding partner of the Community Health Roadmap, which laid the foundation for the recently introduced Community Health Delivery Partnership (CHDP), a country-led partnership to accelerate community-based primary health care and build strong, resilient and inclusive health systems.
HOW TO HELP
There are many ways to make a difference
War, famine, poverty, natural disasters — threats to the world's children keep coming. But UNICEF won't stop working to keep children healthy and safe.
UNICEF works in over 190 countries and territories — more places than any other children's organization. UNICEF has the world's largest humanitarian warehouse and, when disaster strikes, can get supplies almost anywhere within 72 hours. Constantly innovating, always advocating for a better world for children, UNICEF works to ensure that every child can grow up healthy, educated, protected and respected.
Would you like to help give all children the opportunity to reach their full potential? There are many ways to get involved.